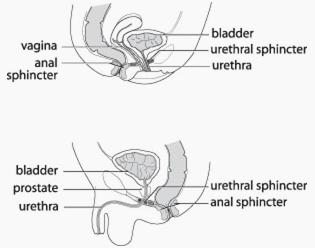
Body waste products are flushed out in the urine and stool. Urine is produced in the kidneys and then carried through long narrow tubes, the ureters, into the bladder. It is stored in the bladder until emptied through its outlet, the urethra. During emptying, the outlet control muscle (urethral sphincter) should relax completely while the bladder contracts to expel urine. Solid waste and unabsorbed food is eliminated in the stool.
In infants, the bowels and bladder empty by reflex. When full, the bladder or bowel empty automatically. Normally, a child gains control of bladder and bowel function by three years of age. A child's bladder normally fills and empties four to six times daily. Bowel movements usually occur every day or two.
Daytime control of urine usually occurs by the age of three with nighttime control occurring a bit later. Some children have persistent bedwetting for several more years, but most will be dry by the age of seven.

Children with abnormal voiding (urine elimination) or defecation (bowel elimination) habits are felt to have a dysfunctional elimination syndrome. The cause of this condition is unknown. These children may be prone to urinary accidents during the day (diurnal enuresis) or night (nocturnal enuresis), bowel accidents (encopresis) or urinary tract infections (UTIs).
Some children will have an overactive bladder with intense urges to void, frequent urination and wetting associated with these urges. You may notice your child dancing or squatting in an effort to suppress urges to void and prevent wetting.
Others resist the signal to void and may do so only two or three times daily. These children may develop an overstretched bladder which cannot contract and empty effectively resulting in wetting or infection. This may be described as a “lazy bladder”.
In some cases, a child may not be able to relax the urethral sphincter completely when trying to void. The partially closed sphincter causes resistance to bladder emptying, high bladder pressure and incomplete voiding, which often leads to wetting or infection. Rarely, high bladder pressure may lead to kidney damage. Some children may have elements of several voiding dysfunctions at once.
In infants, the bowels and bladder empty by reflex. When full, the bladder or bowel empties automatically. Normally, a child gains control of bladder and bowel function by three years of age. A child’s bladder normally fills and empties four to six times daily. Bowel movements usually occur every day or two.
Bowel function may also be a problem in children. Constipation in a child may be indicated when bowel movements occur less than every other day, the stool is large or very hard. Bowel accidents may be a sign of severe constipation.
A child who is constipated will often tense the pelvic floor muscles to avoid stool accidents. These muscles also control bladder emptying and, as a result, bladder function may be affected. For this reason, urinary infection and wetting may be related to constipation. Bladder and bowel problems often occur together and must be treated together.
Our assessment is the first step toward making a diagnosis and developing a treatment plan. Your child’s bladder and bowel habits will be reviewed in detail. A voiding diary, recording times and amounts of urine voided, often will provide useful information. Physical examination may be helpful to uncover an underlying physical problem. We may recommend other investigations, as necessary.
Ultrasound may clarify a child’s internal anatomy. In boys, a bladder examination by X-ray (voiding cysto-urethrography or VCUG) may be required to identify obstruction of the bladder outlet. Spinal X-rays or magnetic resonance imaging (MRI) may be used to identify rare abnormalities of the spine or spinal cord. A bladder pressure study (urodynamic assessment) may provide additional useful information.
The aim of treatment for dysfunctional elimination is to normalize bladder and bowel function, decreasing or preventing daytime and nighttime urine accidents, bowel accidents and infection. Often, a prolonged course of treatment (months to years), requiring ongoing parental patience and support, is necessary to ensure success.
The treatment will generally involve ensuring that your child is drinking adequate amounts of fluid and consuming a balanced diet with plenty of fruit, vegetables and fibre. Such a plan should give your child a healthy foundation for the future and promote proper bowel evacuation.
The child with a lazy bladder should be encouraged to void regularly, every two to three hours, to prevent bladder overfilling. The bladder should be emptied immediately upon getting up in the morning and at bedtime every night.
If your child has an overactive bladder, a bladder relaxant medication, such as oxybutynin (Ditropan™) or tolterodine (Detrol™), may decrease the urge to void and increase bladder capacity.
A child can learn to relax the pelvic floor muscles and sphincter at the time of voiding with the aid of biofeedback which may be available at your hospital or through a physiotherapist. Rarely, a child psychologist may help to focus your child’s attention on the task at hand.
Recurrent infection can be prevented safely with a low dose of antibiotic daily. When bowel function does not improve with dietary measures alone, a stool softener such as docusate sodium (e.g. Colace™) or mineral oil (e.g. LansoÿL™) may be useful.
The good news is that most children overcome their dysfunctional elimination problem. In the vast majority, there is no permanent damage to bladder, kidney or bowel function. The condition can be frustrating for parents and children given that improvement proceeds slowly. Your encouragement and support will go a long way toward helping your child learn to void and defecate normally.