An undescended testicle (cryptorchidism) is a condition which affects about 4% of newborn boys. The testicles, where male hormones and sperm are produced, begin their development in the abdomen next to the kidneys. With growth before birth, they normally descend through the groin into the scrotal sac.
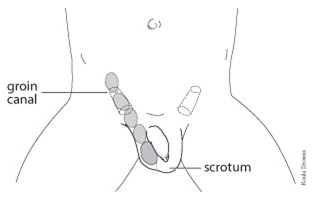
In some boys the descent of one or both testicles is incomplete, with the testicle coming to lie somewhere along the course of its descent from the abdomen to the scrotum. This is often detected by physical examination shortly after birth.
Testicular descent from retroperitoneum to scrotum
An undescended testicle may come down on its own in the first few months of life. In general, such spontaneous descent does not occur after one year of age at which point we will likely recommend treatment to bring the testicle into the scrotum.

Infertility (difficulty fathering children) has been associated with undescended testicles. The risk of infertility is minimal if only one testicle is undescended and more significant if both are affected. Fertility potential may be improved when the testicle is brought down to the scrotum before two years of age.
Undescended testicles are often associated with hernias, which may allow bowel to move from the abdomen through the groin into the scrotum. These hernias are routinely repaired when the testicle is brought into the scrotum surgically.
An undescended testicle slightly increases the risk of testicular tumour development after puberty. These rare cancers are more common in men who have had an undescended testicle. Bringing the testicle into the scrotum does not decrease the risk of cancer developing, but it does allow its earlier detection by examination of the testicle. The earlier such a tumour is detected, the greater the chance of cure.
An undescended testicle is more prone to injury, particularly when located in the groin. Finally, the normal appearance of two testicles in the scrotum may be important for a boy’s self-esteem, particularly at puberty. For all of these reasons, it is important that an undescended testicle be corrected.
When physical examination locates an undescended testicle, usually in the groin, no other investigation is usually necessary. If the testicle cannot be located, it must be determined whether or not it is present. In some boys, a testicle does not develop at all; in others, it may shrivel up before birth often due a disruption of its blood supply.
Ultrasound examination may identify a testicle in the groin or abdomen. In some cases, the abdominal cavity is inspected with a scope passed through the navel under anesthesia (laparoscopy) to localize a testicle undetectable by other means.
Surgical correction of an undescended testicle (orchiopexy) is usually recommended before two years of age. This outpatient operation requires a general anesthetic (the child is put to sleep). A small incision is made in the groin and the testicle is freed up from its tethering attachments. In some cases, this operation can be carried out laparoscopically. Occasionally, the testicle is found to be poorly developed in which case it is best removed. An artificial testicle may be placed in the scrotum after puberty, if appropriate, to produce a more normal appearance.
Front view of lower abdomen, genitalia and upper thighs with inguinal and scrotal incisions
When encountered, a hernia is repaired. We then makes a small incision in the scrotal sac to make room for the testicle. After the testicle is placed in the scrotum, the two incisions are closed with dissolving sutures. A dressing may be placed over the incisions, and your child will be discharged from hospital once he recovers from the anesthetic.
Surgery is successful in over 90% of cases. In some cases, damage to the testicular blood supply may cause the testicle to shrink or fail to grow. Occasionally, a testicle brought into the scrotum surgically will slide back up into the groin, usually in the first few weeks after the operation. A second procedure may be necessary to correct this problem.
It is important to remember that after surgery there is still a risk of developing a testicular tumour despite a successful operation (although the chances of this are still low). A family doctor or pediatrician should examine the child's testicles periodically. All teenage boys should be taught to perform regular testicular self-examination.