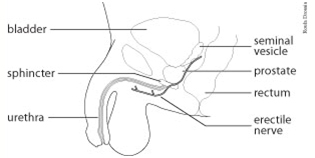
The prostate is a gland wrapped around the urethra, the urine channel, between the bladder and its control muscle, the urethral sphincter. Its main function is to produce part of the semen ejaculated at male orgasm. Each vas deferens carrying sperm from the testicles connects to the prostate. The nerves carrying signals to produce erections run on either side of the prostate.
Cancer may develop in the prostate from which it can grow into surrounding tissues or spread to other parts of the body. Microscopic examination of prostate biopsies confirms the suspicion of cancer and allows some prediction of the tumour's expected behaviour. This is known as the tumourgrade or Gleason score.
Additional investigations may be performed, when necessary, to determine the extent or stage of the cancer. If prostate cancer appears to be confined to the prostate, there are several treatment options available including:
Each option has its own advantages and risks.
Radical prostatectomy involves the complete removal of the prostate and its attached semen glands, the seminal vesicles, with the aim of curing prostate cancer. This option is appropriate for men with localized prostate cancer, good general health and a life expectancy of at least ten years.

Preoperative laboratory tests will be obtained as necessary. In some cases, it may be possible to collect and store your own blood, reducing need to use donated blood if transfusion is necessary.
A “bowel prep” may be recommended before your surgery. The prostate is pressed against the bowel. Stool spillage from a bowel injury during surgery would cause serious problems which often can be prevented by cleansing it of stool. We will instruct you on the form of bowel prep required. This may involve drinking a cleansing solution, taking antibiotic tablets and/or enemas.
It is best to stop taking aspirin, ibuprofen, blood thinners and any vitamin or herbal supplements for at least one week before surgery to reduce the risk of bleeding and unexpected drug interactions. Other medications should be continued as usual.
Most men are admitted to hospital of the morning of surgery. Radical prostatectomy normally is performed under general anesthesia (one is “put to sleep”). In some cases, an epidural anesthetic is used. This involves placing a small plastic tube into the lower back through which medication is given to block painful sensation.
There are several surgical approaches to remove the prostate. Commonly, an incision is made in the lower abdomen below the navel for an open prostatectomy, or small incisions in the abdomen are made for a laparoscopic procedure. When the PSA blood test or biopsies suggest that the cancer has high risk features, pelvic lymph nodes may be removed for immediate examination. In the presence of cancer in these lymph nodes, cure of prostate cancer by radical prostatectomy is not likely. Surgery then may be aborted in favour of other forms of treatment. In the absence of obvious tumour spread, the prostate is exposed and freed from surrounding structures. The urethra is divided below the tip of the prostate preserving as much of the sphincter control muscle as possible. The prostate and seminal vesicles are separated from the bladder and removed. An attempt to spare the erection nerves may be made, unless this could risk leaving cancer behind.
The urethra is sutured to the bladder neck over a catheter passed through the penis into the bladder and held in by a small balloon. This catheter must remain in place until removed as directed by your surgeon.. The abdominal incisions are closed with stitches or metal staples. The operation usually takes two to three hours to complete.
After the Surgery After surgery a catheter through the penis will be left to drain the bladder and a drain will be placed in the lower abdomen to draw off any fluid from the surgical site. Over a few days, these tubes, with the exception of the bladder catheter, will be removed as recovery progresses.
Excellent post-operative pain control may be achieved by several means. This may include using an epidural catheter in the back through which pain killers are administered continuously for a few days. As an alternative, a patient-controlled analgesia (PCA) pump can be used to safely give a small dose of intravenous pain killer at the touch of a button by the patient. These techniques may be supplemented with other medications given by injection, tablet or suppository.
It often takes several days for bowel function to return to normal after any major surgery. Diet will be restored slowly over several days starting with liquids and progressing to solid foods.
Discharge from hospital usually occurs within a few days.
Home visits by a Home Care Nurse may be arranged if deemed necessary. The timing and arrangements for bladder catheter removal are made by the physician usually within a few weeks after surgery.
Any major surgery, including radical prostatectomy, has associated risks. In the short term, bleeding may require blood transfusion and infection may require the use of antibiotics. The stress of surgery may lead to heart or lung problems. Blood clots forming in the legs can be life-threatening if the clots travel to the lungs. Great effort is made to prevent these and other complications.
In the longer term, many men having a radical prostatectomy will lose the ability to have natural erections. Today, several forms of treatment are available to restore erections if this becomes necessary. While the feeling of orgasm usually is preserved, ejaculation will be dry following removal of the prostate and semen glands and the absence of sperm will make one infertile.
Many men will have some degree of urinary leakage after a radical prostatectomy. In most cases this will improve in time with exercises. Some men, however, will have ongoing leakage for which protection in the form of pads may be necessary permanently. Rarely, additional surgery may be required to restore control.