Hormone therapy for prostate cancer involves removing or blocking the male hormone to help control the disease.
Prostate cancer is an abnormal growth of cells originating in the prostate gland. These abnormal cells may spill out of the prostate into surrounding tissues or spread to other parts of the body, most often into lymph nodes or bones. Hormone therapy is a treatment method used to control prostate cancer in an effort to relieve or prevent symptoms and maximize life expectancy.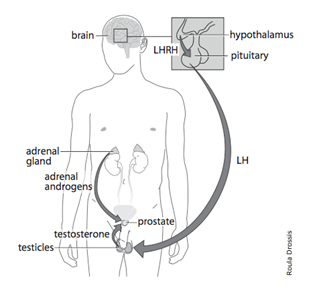
Hormones are natural chemical messengers produced by various glands to control body functions. The testicles produce testosterone which is the major male sex hormone (androgen). The release of testosterone is controlled by another hormone produced in the brain called luteinizing hormone releasing hormone (LHRH). Small amounts of additional androgens are produced in the adrenal glands located above each kidney.
Male with LHRH controlling the release of testosterone from the testes

Hormonal control of prostate cancer can be accomplished in several ways. Given that androgens are produced primarily by the testicles, their surgical removal (orchiectomy) will effectively achieve the desired effect. This minor surgical procedure, usually performed in the hospital on an outpatient basis, involves removal of the testicles through a small incision in the scrotal sac. There is usually little pain post-operatively and the risk of infection, swelling or bruising is small. Most men are able to resume their usual activities within a few weeks.
Some men prefer to have the testicles suppressed rather than removed. This can be accomplished with a drug which specifically blocks the release of LHRH by the brain which is necessary for testosterone production. This medication, an LHRH analog(e.g. buserelin, goserelin or leuprolide), is administered by injection at regular intervals (usually every one to six months). It is important to receive these injections on time according to the schedule recommended by your doctor. LHRH agonist treatment and orchiectomy are equally effective for prostate cancer control.
Several medications taken by mouth can block the effect of androgens without suppressing their production. These drugs called anti-androgens (e.g. bicalutamide, flutamide or nilutamide) may by used alone or in combination with an LHRH agonist or orchietomy. They are often used prior to starting the LHRH agonist injections to block a short-lived increase in testosterone production caused by the first injection. Once the injections have completely suppressed the androgens from the testicles, the anti-androgens medications can often be stopped. Some studies suggest that continuing the anti-androgen with the LHRH agonist injections may improve cancer control (total androgen blockade).
The effect of hormone therapy is monitored with regular review of health status, examination of the prostate and testing the PSA level, which usually falls with effective prostate cancer control.
Male hormones serve several important functions in the body. Their elimination, by surgery or medication, may result in a number of effects. Most men will have hot flushes, much like those experienced by women at menopause. The frequency and severity of hot flushes are variable and, often, they decrease over time.
Androgens are necessary to maintain sexual drive and performance. Men on hormone therapy often lose interest in sex and have difficulty with erections. Fortunately, effective treatment is available to restore erections for those in whom this is important.
Mild anemia (low red blood cell count) is common and may contribute to a slight loss of energy or fatigue. Muscle strength may decrease. Thinning of the bones (osteoporosis) may lead to an increased risk of fractures. In some cases, this risk can be reduced with calcium and vitamin D supplements or with the use of additional medications (bisphosphonates). Side effects of anti-androgens may include nausea, diarrhea, breast tenderness and liver dysfunction.
Both having cancer and hormone therapy may cause a slight increase in the risk of blood clot formation which could lead to a stroke or heart attack.
While treatment should be started promptly for any man with symptoms due to prostate cancer (such as disease that has spread into the bones), the timing of hormone therapy in men without symptoms remains controversial. Some believe that hormone therapy should be started at the first sign of disease activity (usually a rising PSA) before symptoms develop (early treatment). Others feel that treatment can be delayed for months or even years (deferred treatment) without great risk. Studies are underway to determine the optimal timing of hormone therapy.
Although hormone therapy is usually used continuously, some men prefer intermittent hormone therapy. An LHRH agonist is given for a specified period (often up to one year) until the PSA level and cancer are maximally suppressed. Treatment is then stopped to allow testosterone production to resume and the side effects of the medication to disappear (which may often take months). The cancer can be expected to become active slowly over the next months as indicated by a rising PSA. Treatment is restarted when the PSA level or tumour growth suggests that re-suppression is required. This strategy of cyclic treatment aims to balance cancer control while minimizing treatment side effects.
In some cases, hormone therapy may be used in combination with other forms of treatment (adjuvant hormone therapy). Hormone therapy can be given before or after radiation treatment in some patients in order to help mop up more of the cancer cells. A similar approach is used by us prior to surgical removal of the prostate.
Hormone therapy is an effective way of controlling prostate cancer often resulting in symptom-free and rewarding life for years.